
COVID cases are rising again, as EG.5 is spreading quickly, and BA.2.86 has mutations that may make it more transmissible (studies are underway). “COVID vaccines, tests and effective treatments are helping keep people out of the hospital,” says UC Davis Health. “Still, this uptick in COVID-19 cases is a good reminder to follow CDC recommendations, wash your hands and stay away from sick people. And if you’re sick, stay home to avoid spreading it to others.” It’s also the best time to know the “first signs” of catching any of these COVID variants. “You should look for the following COVID symptoms,” says UC Davis Health.

“The coronavirus strain nicknamed ‘eris; was responsible for more than 1 in 5 new infections in recent weeks, according to updated data from the Centers for Disease Control and Prevention,” says U.S. News and World Report. “EG.5, or ‘eris,’ is the top strain circulating in the U.S., causing nearly 22% of cases over the past two weeks, according to CDC data. The strain has been increasing in recent weeks as XBB.1.5 declines. EG.5 appears more transmissible and better able to evade immunity provided by vaccines and previous infection, according to WHO. But it hasn’t been associated with more severe disease.”A fever is the most common symptom of COVID.

A persistent cough is another symptom of EG.5. Doctors say those suffering from a cough should stay hydrated, gargle with warm salt water, and use cough lozenges to take the edge off. “The best approaches are typically what grandma would advise,” says Dr. Michelle Prickett, a pulmonology and critical care specialist at Northwestern Medicine.

EG.5 may present as a very sore throat, similar to a cold. “People… have reported having a sore throat that feels similar to what you might experience during a cold, giving a ‘scratchy’ or irritated sensation,” according to the ZOE study app about COVID variants. “COVID-related sore throats tend to be relatively mild and last no more than five days. A very painful sore throat that lasts more than five days may be something else, such as a bacterial infection, so don’t be afraid to contact your GP if the problem persists.” They add: “It’s important to remember that sore throats are common and caused by lots of respiratory illnesses such as normal colds. So although many people with COVID-19 experience sore throats, most people with a sore throat will not have COVID-19.”

A runny nose is another symptom of EG.5, similar to previous subvariants. “During the [2021] winter wave, we noticed that a runny nose was the second most commonly reported symptom in the app after headaches,” says the ZOE study app. “And nearly 60% of people who tested positive for COVID-19 with loss of smell also reported having a runny nose. While symptoms like cough, fever and loss of smell are common in those who test positive for COVID-19, we found that having a runny nose and sneezing was only very slightly more common in people who tested positive for COVID-19 than those who tested negative.”
So, short of getting tested, how likely is a runny nose to be linked to COVID? “Our data shows that when rates of COVID-19 are high, the chances that a runny nose is due to coronavirus infection is high. But when rates of COVID-19 are low, it’s less likely to be a symptom and more likely to be due to another cause such as a cold or allergy.”

Early in the pandemic, Dr. Sanjay Gupta mentioned that studies had found that nearly half of early COVID patients in Wuhan, China, reported digestive symptoms as one of the first signs of their illness, including diarrhea, abdominal pain, vomiting, and loss of appetite. “Sometimes the early symptoms aren’t these classic symptoms,” he said.

“Loss of smell—anosmia—seems to be another symptom that any of these patients often develop,” said Gupta. “They don’t know if it’s related to the upper respiratory virus part of this or what but anosmia, maybe linked to loss of taste, maybe linked to loss of appetite. We’re not entirely sure, but it’s clearly something to look out for.”

Gupta reported on one 47-year-old man who was healthy and fit, but found himself hospitalized with COVID, “with a left lung filled with blood clots and a brain stuck in a deep fog. Indeed, he felt like he was losing his mind. The splitting headaches and overwhelming fatigue convinced him his brain was on fire.”
COVID can cause a raft of neurological problems. “Although estimates vary, studies have found that at least half of people who recover from COVID-19 continue to suffer from neurological symptoms for months after,” wrote Gupta. “Brain scans of patients, compared with scans of those who’ve never been infected, show structural and functional changes to the brain.”

Coronavirus affects your nervous system, which is in charge of keeping your body balanced, steady, and stable. While most COVID-19 patients present with common symptoms such as fever or cough, many also complain of dizziness while fighting the virus.
“Neurological symptoms caused by COVID‐19 are diverse and complex,” according to a study published in The Journal of the American College of Emergency Physicians Open. The study authors also claim, “Non‐specific symptoms including headache, dizziness, vertigo, and paresthesia have been reported.”

Another symptom that’s been found among COVID-19 patients is itchy skin or skin that develops rashes or lesions. A study published in JAMA Dermatology analyzed four coronavirus patients and the changes that occured in their skin.
“The patients had skin findings of acral fixed livedo racemosa and retiform purpura,” the study found. This means the coronavirus patients’ skin was discolored and developed lesions, possibly from the effects the virus has on the circulatory system. So far, this symptom has only been reported in severe COVID-19 cases.

If you’re feeling a little confused, it may be a symptom of COVID-19. The virus has been known to affect the brain, according to Dr. Robert Stevens, M.D. from John Hopkins University. Confusion may be a side effect of coronavirus due to low blood oxygen levels or other effects on the neurological system. Dr. Stevens estimates that “at least half of the patients I’m seeing in the COVID-19 units have neurological symptoms.”
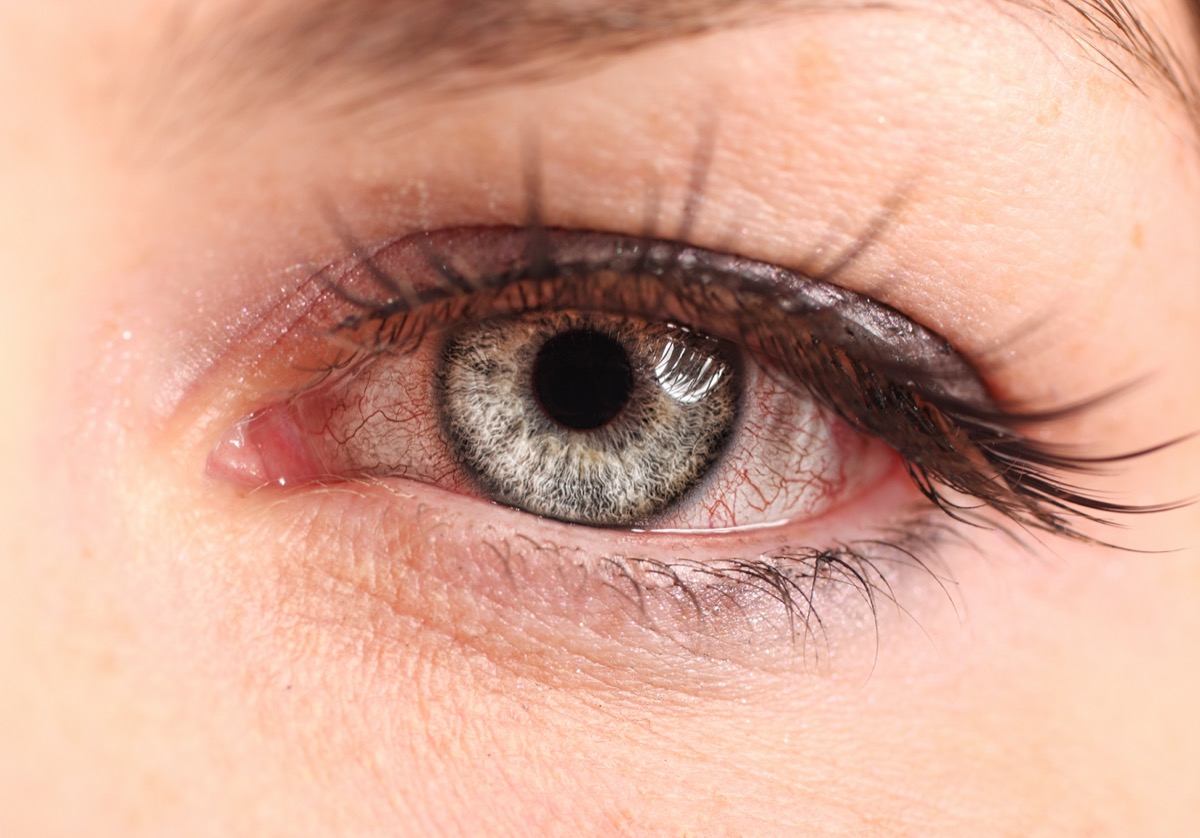
The eye problems associated with COVID-19 are more likely to occur in patients with severe cases of the virus. These eye-related symptoms may include “enlarged, red blood vessels, swollen eyelids, excessive watering and increased discharge,” according to the Mayo Clinic. Some coronavirus patients also reported light sensitivity or general eye irritation.

Gastrointestinal symptoms are becoming more common among COVID-19 patients, with a loss of appetite being reported in addition to nausea or diarrhea. A study conducted by Stanford Medicine analyzed symptoms of 116 COVID-19 patients who were admitted to the hospital. The most common presenting symptom was a cough but the study found that “gastrointestinal symptoms were reported by 31.9% of patients” and 22.3% of these patients reported a loss of appetite.

Some medical experts have found that COVID-19 patients are experiencing silent hypoxia. This occurs when the patient measures for a dangerously low blood oxygen level but doesn’t experience shortness of breath. In most cases, patients originally sought treatment due to other more common symptoms, such as fatigue or cough.
There are many theories as to why the virus causes these low blood oxygen levels without shortness of breath. “One theory is that the virus may affect the airways of the lungs as well as the blood vessels flowing through the lung,” according to American Lung Association’s Chief Medical Officer, Albert Rizzo, M.D.

COVID toes are described as “a painful or itchy skin rash that sometimes pops up in young adults with otherwise mild or asymptomatic cases of COVID-19,” by the University of California San Francisco. Also commonly referred to as “chilblains,” you can identify this foot condition with purple discoloration, dryness, or rash on the toes.
COVID toes can also be splotchy or show up as red dots. Coronavirus patients who suffer from COVID toes report the condition as being painful and itchy, sometimes making it hard to walk.

Abnormal blood clotting is a newly developed side effect that’s been reported in some COVID-19 patients. A study published in Blood analyzed 400 COVID-patients who were hospitalized. It found that 10% of the patients experienced blood clotting and most of the cases were deep vein thrombosis. This condition occurs when a blood clot forms deep within the veins of your body, mainly your thighs or lower legs.
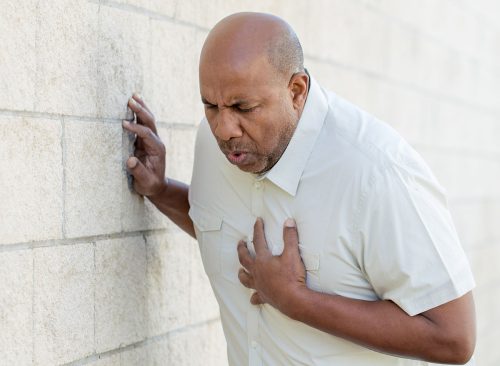
Shortness of breath is one of the CDC’s main coronavirus symptoms but tightness in the chest may also need to be added to the list. Tightness in the chest may be caused by coronavirus attacking the respiratory system.
“After gaining entry through either the nose or mouth, the virus travels to the chest and begins to cause injury to the respiratory system,” according to Dr. Tim Connolly from Houston Methodist. Some COVID-19 patients fully recover from the damage to their airways while more severe cases may see long-term damage.

When you get sick with a regular cold or flu, you may find your vision blurs due to the fever or effects the illness has on your nervous system. With COVID-19, some patients reported experiencing blurry vision, which may be a side effect of their immune system fighting off the virus. A study published in JAMA Ophthalmology analyzed 38 COVID-19 patients in China and found that 31.6% experienced some type of eye-related ailment while recovering from the virus.

Cardiac problems aren’t related to COVID-19 as a presenting symptom, but the virus may cause damage to the heart and circulatory system in patients with severe cases. A study published in JAMA Cardiology examined 100 coronavirus patients who sought medical treatment for the virus.
After studying the patients’ cardiac magnetic resonance (CMR) imaging, the study found that 78 patients had some type of heart involvement and 68 had active cardiac inflammation. Study authors believe the virus may exacerbate underlying heart conditions and specific cardiac problems are related to the severity of the COVID-19 case.

The CDC warns that muscle aches are a symptom of COVID-19 but many patients also report muscle weakness after contracting the virus. When your immune system is in full force, inflammation usually occurs in the body, which may be why muscle weakness is associated with COVID-19. Patients who are hospitalized for severe cases may experience “skeletal muscle injury due to the direct effects of the virus,” according to a study published in Cureus.

Throughout the pandemic, the CDC has been adding to the list of the most common symptoms. It seems the experts have narrowed it down to 11 common symptoms, which most infected individuals begin to feel two to 14 days after exposure to the virus. These symptoms include:
- Fever or chills.
- Cough.
- Shortness of breath or difficulty breathing.
- Fatigue.
- Muscle or body aches.
- Headache.
- New loss of taste or smell.
- Sore throat.
- Congestion or runny nose.
- Nausea or vomiting.
- Diarrhea.
These are the most common presenting symptoms and many individuals infected with COVID-19 experience one or more of these symptoms after exposure to the virus. However, these aren’t the only symptoms you could experience if you catch COVID-19.

Dr. Li says, “The biggest threat today with COVID is the unpredictable development of Long COVID. This is the sequela of more than 100 different symptoms ranging from mild to disabling resulting from COVID infection. Long COVID may last for months or in some cases even years. It remains difficult to pin down, and there is no cure. People with long COVID may even become disabled and unable to work or engage in activities of daily living.
There is emerging evidence that past COVID infection, even when mild, can lead to the increased risk of heart attack, stroke, diabetes, and Alzheimer’s disease. These have been unexpected consequences that signify COVID is a serious disease. Researchers may be years away from having a deep understanding of Long COVID, already it’s known that Covid infection can lead to long-term damage to small blood vessels, nerves, and it can trigger autoimmune and chronic inflammation for all of these reasons, Covid remains a serious illness that merits society to remain cautious and to take precautions.”

Dr. Li explains, “Long COVID is a second illness that mysteriously appears in some people after they recover from an acute infection of COVID. While most people experience relatively mild symptoms from acute COVID now, especially those who are vaccinated and boosted, long COVID can appear as a bewildering group of sometimes severe symptoms. The symptoms of long COVID range from extreme fatigue, shortness of breath, racing heart, brain, fog, abdominal discomfort, muscle and joint pain, ringing of the ears, and more than 100 other symptoms have been described.
The symptoms can occur in up to 30% of people who have had COVID, but so far, it’s not known who is likely to develop long COVID. At present, there is no cure for long COVID and some people have suffered for more than one year. And when the symptoms are serious, they can be disabling and interfere with the ability to work, and even activities of daily living. Long COVID can comprise one’s quality of life. People with long COVID qualify for benefits under the American Disabilities Act.”

According to Dr. Li, “There are more and more symptoms emerging that are associated with COVID infection that qualify under the term long COVID. The most significant are extreme fatigue, and neurological symptoms like brain fog. The cardiovascular symptoms can also be significant, and there’s an increased risk of heart attack, arrhythmias, and heart failure as part of a continuum of long COVID. There are also reports showing an increased risk for the development of new onset, diabetes, and new onset Alzheimer’s disease after COVID infection.”
The American Stroke Association states, “The possible long-term effects include “a myriad of symptoms affecting different organs,” said Dr. José Biller, director of the COVID-19 neurology clinic at Loyola Medicine in Maywood, Illinois. “So, it could be the lungs, it could be cardiovascular, it could be the nervous system, it could be mental health or behavioral problems.”
The Mayo Clinic lists the following uncommon signs to be aware of.
Eye Problems
“Pink eye (conjunctivitis) can be a COVID-19 symptom. Research suggests that the most common eye problems linked to COVID-19 are light sensitivity, sore eyes and itchy eyes.
Confusion
Severe confusion (delirium) might be the main or only symptom of COVID-19 in older people. This COVID-19 symptom is linked with a high risk of poor outcomes, including death.
Skin Changes
The most common skin changes linked with mild to severe COVID-19 include a flat rash covered with small bumps, discolored areas on the fingers and toes (COVID toes), and hives.
COVID toes appear to be more common in children and young adults. Swelling or discoloration can develop on one or several toes or fingers. The hands, wrists or ankles also can be affected. Blisters, itchiness, rough skin, or painful bumps can occur. A small amount of pus might develop under the skin. The symptoms can last 10 to 14 days or for months.
However, swollen, discolored fingers or toes could also be chilblains, an inflammatory skin condition. Chilblains develop in response to repeated exposure to cold air.”

Experts caution that vaccines and boosters are still the best way to prevent serious illness. “Certainly there have been tremendous waves of infection with each different variant, but to a large degree, the vaccines have held their protection against severe disease,” says Alessandro Sette, a professor at the La Jolla Institute for Immunology. “Now we have bivalent boosters that are even better—that’s very important.” Sette emphasizes that although XBB.1.5 is more immune-evasive than other variants, it can’t escape the immune system completely, especially when it comes to the cellular immunity conferred by killer T cells, which destroy cells infected by virus.
Paxlovid and other antiviral COVID treatments such as remdesivir “should still be effective.”

Mask up in places of high transmission, said Dr. Anthony Fauci this weekend. “I am concerned that people will not abide by [masking] recommendations,” Fauci said. “We’re not talking about mandates or forcing anybody, but when you have a situation where the volume of cases in society gets to a reasonably high level, the vulnerable, the elderly, those with underlying conditions, are going to be more susceptible, if they do get infected, of getting severe disease leading to hospitalization. We know that. That’s a fact,” he said, according to Fortune.
RELATED: 23 Places You’re Most Likely to Catch the New COVID Variant

While there are many common symptoms of COVID-19 that can help you spot the virus, keep in mind, some patients experience no symptoms at all. The CDC estimates that about 40% of people who are infected with the virus are asymptomatic at some point, which may be what’s contributing to the quick and wide spread of infection. If you think you may have been exposed to the virus, it’s best to get tested and self quarantine, even if you don’t feel any symptoms.














